Medicare Part C Eligibility Things To Know Before You Get This
Table of ContentsAn Unbiased View of Medicare Supplement Plans Comparison Chart 2021 PdfThe Greatest Guide To Boomer Benefits ReviewsHow Boomer Benefits Reviews can Save You Time, Stress, and Money.The Only Guide to Medicare Select PlansGetting My Apply For Medicare To WorkAn Unbiased View of Medicare Select Plans
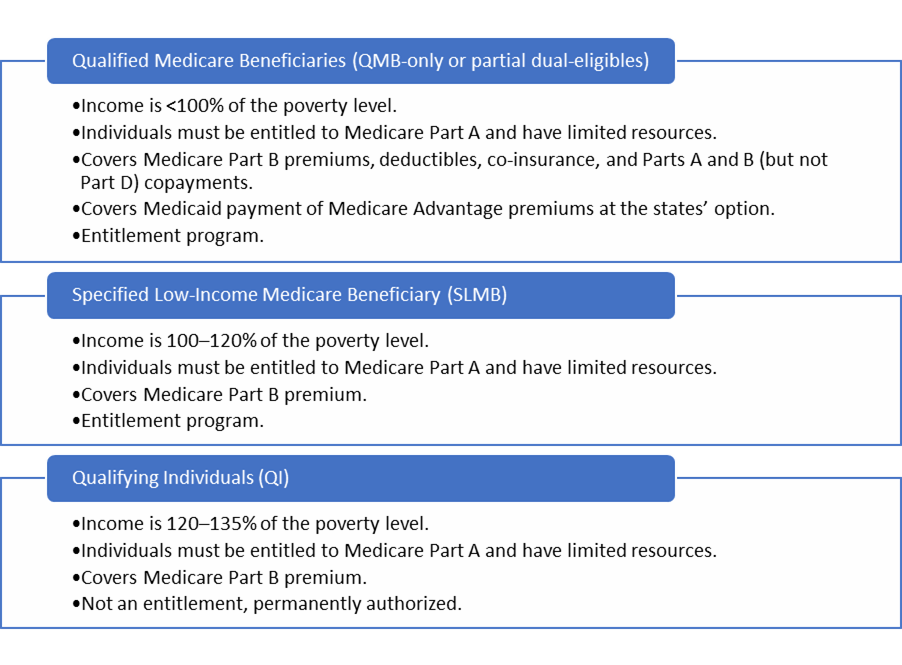
Nelson does not need to submit an application for Premium-Part A since he resides in a Component A Buy-in State. (Note: If Maryland authorizes Mr. Nelson's application for the QMB Program, the State will enlist him in State Buy-in since he already has Component B.
Read listed below to discover out-- If he has Medicaid or QMB, just how a lot will Medicaid pay?!? SHORT RESPONSE: QMB or Medicaid will pay the Medicare coinsurance just in restricted circumstances.
The Buzz on Medicare Part G
This creates stress in between a specific and also her medical professionals, drug stores giving Component B drugs, as well as other suppliers. Carriers might not recognize they are not allowed to bill a QMB beneficiary for Medicare coinsurance, because they bill other Medicare beneficiaries. Even those that know might pressure their people to pay, or just decrease to serve them.
2 (dental and vision insurance for seniors). Exactly how Does a Supplier that DOES accept Medicaid Expense for a QMB Recipient? The copyright expenses Medicaid - even if the QMB Recipient does not likewise have Medicaid. Medicaid is called for to pay the company for all Medicare Part An as well as B cost-sharing charges for a QMB recipient, also if the service is usually not covered by Medicaid (ie, chiropractic, podiatry and also scientific community service treatment).
Cuomo has actually proposed to decrease exactly how much Medicaid spends for the Medicare prices also further (medicare select plans). The quantity Medicaid pays is various depending upon whether the individual has Original Medicare or is a Medicare Advantage strategy, with far better settlement for those in Medicare Benefit plans. The answer also differs based on the type of solution.
The Best Guide To Medicare Select Plans
- - Currently, Medicaid pays the complete Medicare authorized costs up until the recipient has fulfilled the annual deductible, which is $198 in 2020. Dr. John charges $500 for a browse through, for which the Medicare approved cost is $198. Medicaid pays the entire $198, fulfilling the insurance deductible. If the beneficiary has a spend-down, after that the Medicaid payment would certainly be subject to the spend-down.
If the Medicaid rate for the same solution is just $80 or much less, Medicaid would pay nothing, as it would consider the doctor fully paid = the provider has actually obtained the complete Medicaid rate, which is lower he said than the Medicare rate. s - Medicaid/QMB wil pay the full coinsurance for the following services, despite the Medicaid price: ambulance and psychologists - The Gov's 2019 proposal to remove these exemptions was turned down.
Unknown Facts About Medicare Supplement Plans Comparison Chart 2021
50 of the $185 authorized price, service provider will with any luck not be deterred from serving Mary or various other QMBs/Medicaid receivers. - The 20% coinsurance is $37. Medicaid pays none of the coinsurance because the Medicaid rate ($120) is less than the amount the company currently received from Medicare ($148). For both Medicare Advantage as well as Original Medicare, if the costs was for a, Medicaid would certainly pay the full 20% coinsurance no matter the Medicaid rate.
If the copyright wants Medicaid to pay the coinsurance, then the supplier has to sign up as a Medicaid service provider under the state policies. This is an adjustment in plan in implementing Section 1902(n)( 3 )(B) of the Social Safety And Security Act (the Act), as customized by section 4714 of the Well Balanced Budget Plan Act of 1997, which forbids Medicare providers from balance-billing QMBs for Medicare cost-sharing.
This section of the Act is available at: CMCS Informational Bulletin . QMBs have no legal obligation to make further repayment to a copyright or Medicare took care of treatment strategy for Component A or Component B expense sharing. Suppliers that wrongly costs QMBs for Medicare cost-sharing undergo assents. Please keep in mind that the law referenced above supersedes CMS State Medicaid Manual, Chapter 3, Eligibility, 3490.
Medicare Part C Eligibility Fundamentals Explained
See this excerpt of the 2017 phone call letter by Justice in Aging - It can be hard to reveal a company that one is a QMB. It is specifically hard for service providers who are not Medicaid suppliers to recognize QMB's, given that they do not have accessibility to on-line Medicaid qualification systems If a customer reports an equilibrium billng trouble to this number, the Consumer Solution Representative can rise the issue to the Medicare Administrative Contractor (MAC), which will send out a conformity letter to the provider with a copy to the consumer.
Medicaid pays none of the coinsurance since the Medicaid rate ($120) is reduced than the quantity the company already obtained from Medicare ($148). For both Medicare Benefit and Original Medicare, if the bill was for a, Medicaid would certainly pay the full 20% coinsurance no matter of the Medicaid price.
If the service provider desires Medicaid to pay the coinsurance, after that the service provider must sign up as a Medicaid copyright under the state rules. This is a change in policy in carrying out Section 1902(n)( 3 )(B) of the Social Safety Act (the Act), as changed by area 4714 of the Balanced Budget Plan Act of 1997, which restricts Medicare service providers from balance-billing QMBs for Medicare cost-sharing.
Fascination About Medicare Select Plans
QMBs have no lawful commitment to make more settlement to a service provider or Medicare handled care plan for Part A or Part B cost sharing. Service providers who inappropriately costs QMBs for Medicare cost-sharing are subject to permissions.
